- About Us
- Stem Cells
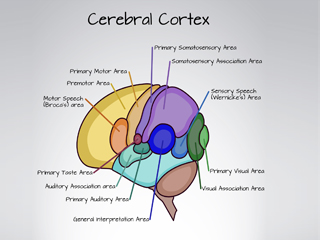
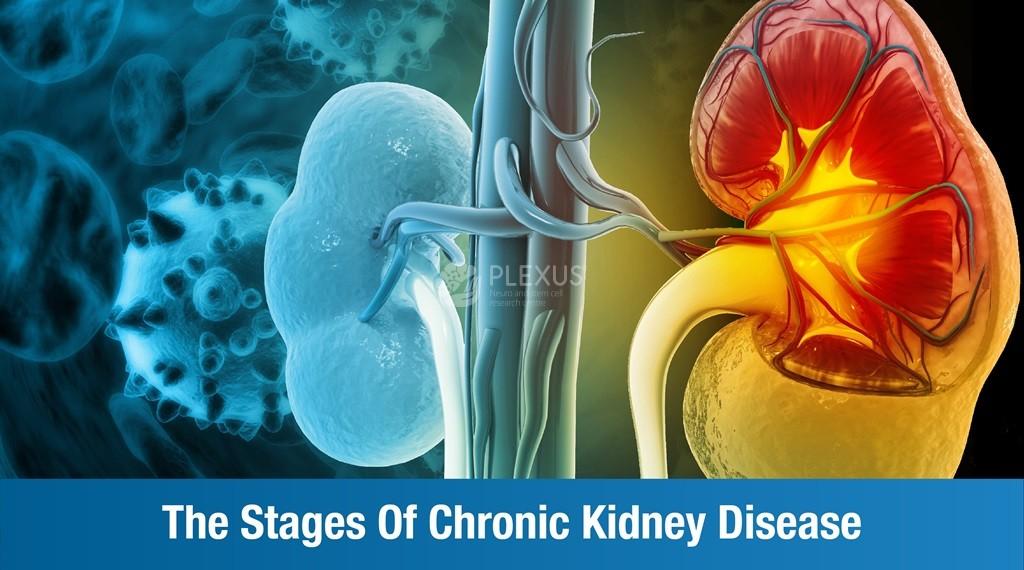
- Neurology
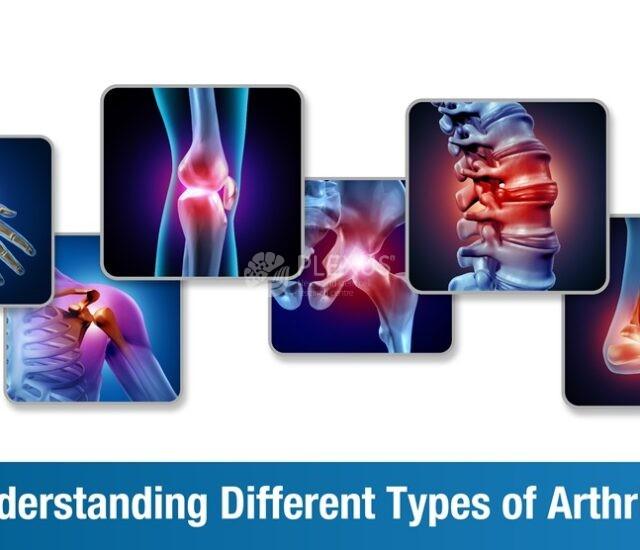
- Disorders
- Services
- All Therapies
- Regenerative Rehabilitation
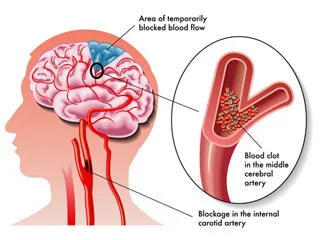
- Rehabilitation for Stroke
- Rehabilitation for Spinocerebellar Ataxia
- Parkinson’s Disease Rehabilitation
- Multiple Sclerosis Rehabilitation
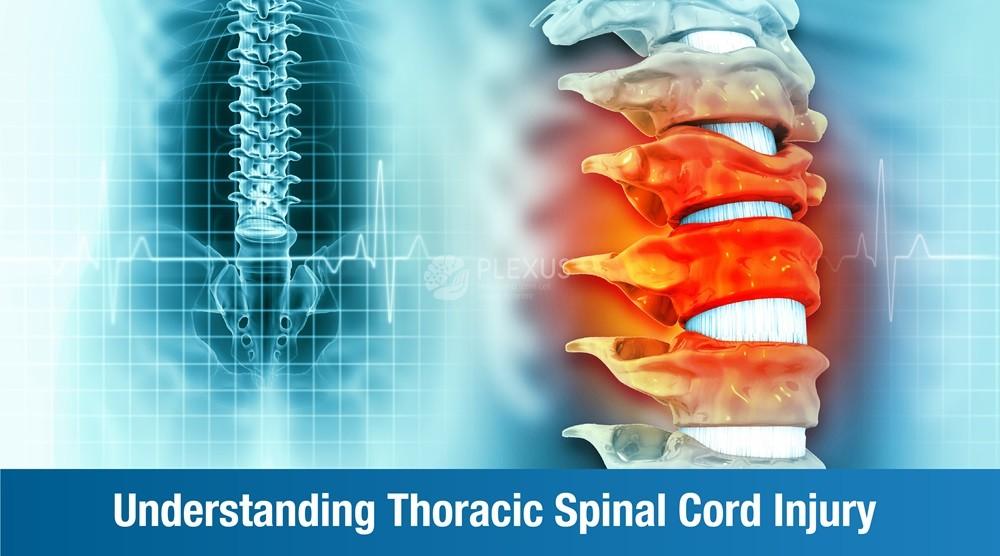
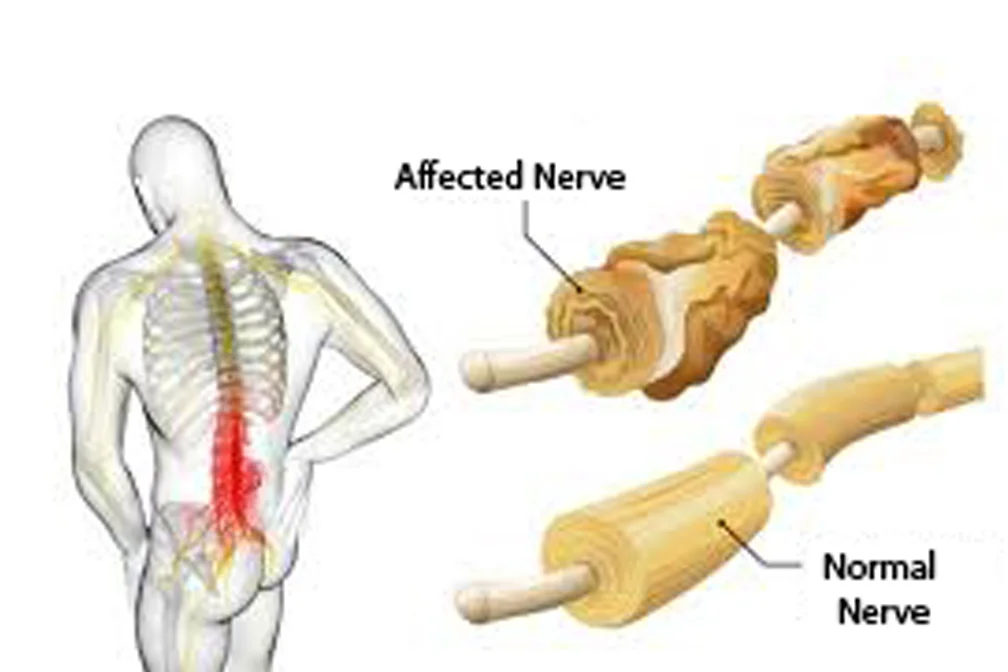
- Rehabilitation for Spinal Cord Injury
- Rehabilitation for Motor Neuron Disease
- Rehabilitation for Cerebral Palsy
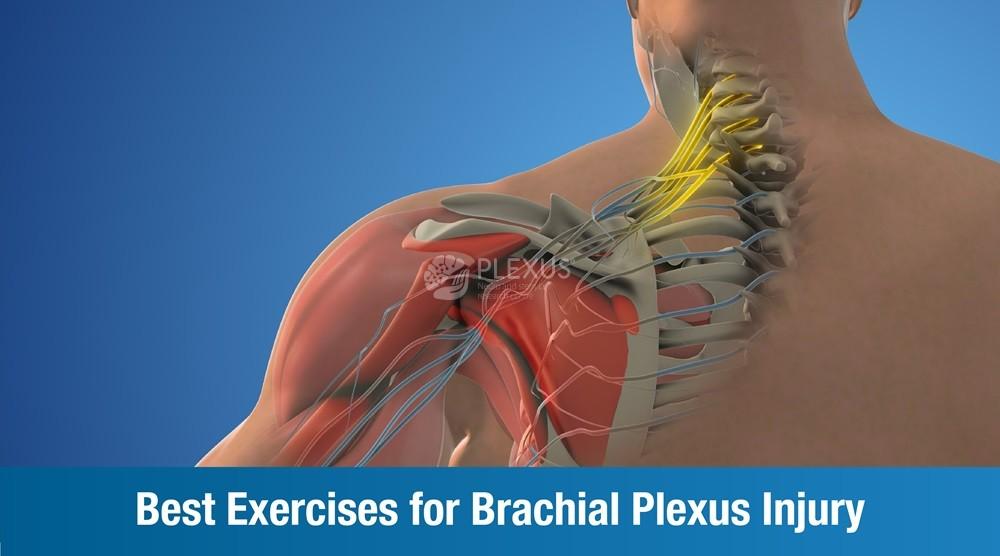
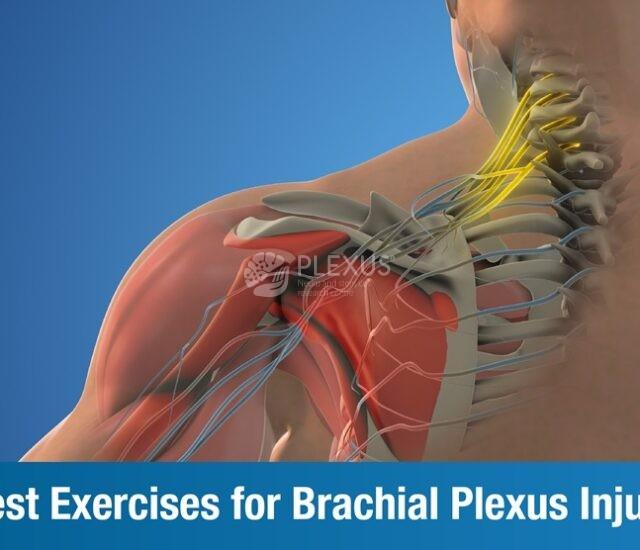
- Brachial Plexus Injury rehabilitation
- Rehabilitation for Global Developmental Delay
- Childhood Disorders Clinic
- Outpatient Services
- Ask a question
- Request an appointment
- About Us
- Stem Cells
- Neurology
- Disorders
- Services
- All Therapies
- Regenerative Rehabilitation
- Rehabilitation for Stroke
- Rehabilitation for Spinocerebellar Ataxia
- Parkinson’s Disease Rehabilitation
- Multiple Sclerosis Rehabilitation
- Rehabilitation for Spinal Cord Injury
- Rehabilitation for Motor Neuron Disease
- Rehabilitation for Cerebral Palsy
- Brachial Plexus Injury rehabilitation
- Rehabilitation for Global Developmental Delay
- Childhood Disorders Clinic
- Outpatient Services
- Ask a question
- Request an appointment